Crohn’s disease, a subtype of inflammatory bowel disease (IBD), presents complex challenges for both patients and practitioners. Despite advanced treatment protocols involving anti-inflammatory medications and tailored dietary plans, many individuals, like Lisa—a 35-year-old woman diagnosed with Crohn’s—continue to experience persistent symptoms, such as abdominal pain, diarrhoea, and fatigue. This raises a critical question: could genetics be influencing the severity and persistence of her disease?
Understanding the Genetic Landscape of Crohn’s Disease
Crohn’s disease is multifactorial, involving a blend of genetic predispositions and environmental triggers. Research has linked specific genetic variants to an increased risk of developing Crohn’s, shedding light on why some patients respond differently to treatment and why their symptoms may persist.
One significant genetic factor in Crohn’s disease is the FUT2 (fucosyltransferase 2) gene. The FUT2 gene plays a crucial role in the secretion of histo-blood group antigens, which are key to determining the gut’s microbial composition. Variations in this gene can dramatically affect gut health and immune responses.
The Role of FUT2 in Crohn’s Disease
The FUT2 gene determines secretor status, which is the ability to secrete blood group antigens into bodily fluids and the gastrointestinal tract. People who are non-secretors—those with inactive FUT2 genes—show a higher susceptibility to Crohn’s disease. Here’s why:
- Altered Gut Microbiota Composition: FUT2 influences the diversity and attachment of gut bacteria by regulating the availability of fucose, a carbohydrate crucial for beneficial bacterial colonization. Non-secretors tend to have altered gut microbiota, characterized by reduced probiotic populations and an increased risk of dysbiosis. This imbalance can contribute to chronic inflammation, a hallmark of Crohn’s disease.
- Impact on Butyrate Production: Butyrate, a short-chain fatty acid with strong anti-inflammatory properties, is essential for maintaining gut health. FUT2 non-secretors often have lower levels of butyrate-producing bacteria, which can exacerbate inflammation in the gut and impair the gut-brain axis. Supplementing with butyrate or enhancing its production could, therefore, play a protective role in managing Crohn’s symptoms.
- Immune Response Modulation: The absence of secreted antigens in non-secretors influences the immune system’s recognition processes. This can lead to compromised immune responses and increased vulnerability to infections. The gut mucosal immunity, a key line of defence in preventing inflammation and infection, is notably affected by secretor status.
Cell Signalling Pathways and Disease Implications
Beyond its impact on gut microbiota, FUT2 is involved in modulating various cell signalling pathways:
- Autophagy and Apoptosis: FUT2 has been shown to promote autophagy (the body’s process of cleaning out damaged cells) and suppress apoptosis (programmed cell death) in certain contexts, such as lung adenocarcinoma.
- Colorectal Cancer Risks: While FUT2 promotes gut health, non-functional FUT2 variants can lead to a higher risk of harmful bacterial colonization, creating an environment that favours inflammation and, in some cases, cancerous developments.
Clinical Considerations for Practitioners
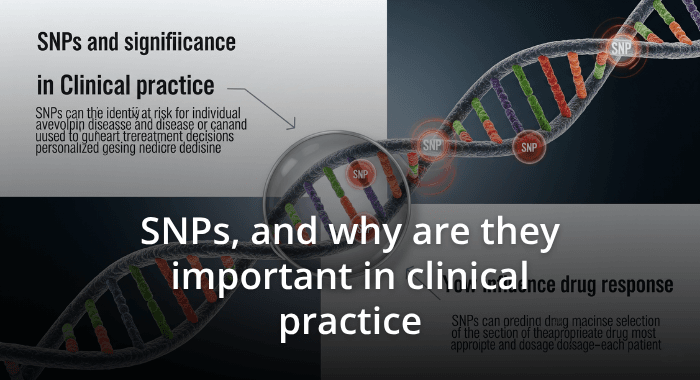
For practitioners managing patients with Crohn’s disease, understanding their genetic predispositions is vital for developing personalized treatment plans. Identifying FUT2 status and other relevant SNPs can guide targeted interventions. For example:
- Assessing Butyrate Levels: Addressing low butyrate production in non-secretors can be an effective therapeutic approach. This may involve dietary changes, prebiotic and probiotic supplementation, and direct butyrate supplementation.
- Tailored Nutritional Strategies: Modifying a patient’s diet to promote gut health and reduce inflammation can have significant benefits. Ensuring an intake that supports a diverse and healthy gut microbiome is essential, especially in patients with compromised fucose availability.
- Monitoring Immune Response: Understanding how genetic variants affect immune response can help practitioners preempt potential complications, such as recurrent infections or heightened inflammation.
Moving Forward: The Future of Genomic Medicine in IBD
The intersection of genetics and environment is the key to understanding the triggers and progression of Crohn’s disease. While we all carry genetic predispositions, it is where these intersect with environmental factors that the disease manifests and progresses. Genetic testing that includes FUT2 and other relevant markers can provide valuable insights and empower both practitioners and patients to develop proactive, personalized treatment plans.
As research in genomics continues to evolve, practitioners are better equipped than ever to explore the underlying genetic factors that impact disease susceptibility and treatment response. For patients like Lisa, this means the hope of more targeted, effective care that addresses not just the symptoms but the genetic roots of their condition.
WANT TO LEARN MORE? Join us at the upcoming Autoimmune and Thyroid Genomics Workshop