The thyroid gland, a butterfly-shaped organ located at the base of your neck, plays a pivotal role in regulating metabolism, energy production, and overall health. Thyroid dysfunctions, such as hypothyroidism, hyperthyroidism, Hashimoto’s thyroiditis, and Graves’ disease, affect millions worldwide. While many factors contribute to thyroid issues, one genetic component gaining attention is the MTHFR gene.
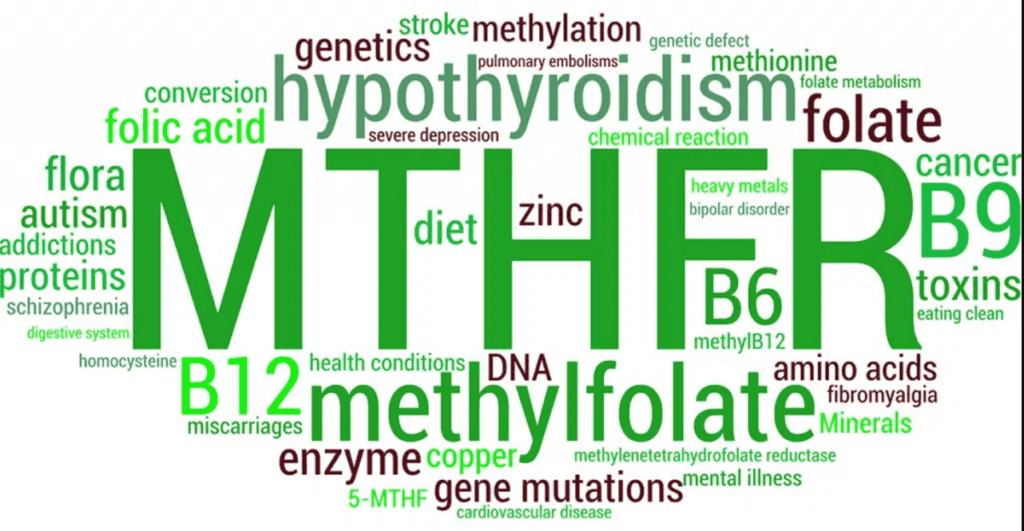
The MTHFR (methylenetetrahydrofolate reductase) gene produces an enzyme critical for methylation, a biochemical process vital for detoxification, DNA repair, neurotransmitter synthesis, and hormone regulation. The interplay between MTHFR mutations (or polymorphisms) and thyroid function is multifaceted, as methylation is essential for the production and activation of thyroid hormones. Let’s explore this connection in detail.
1. Understanding MTHFR Polymorphisms
MTHFR gene mutations can reduce the efficiency of the MTHFR enzyme, leading to impaired methylation. Two common variants of the MTHFR gene are C677T and A1298C. People with these mutations may experience:
- Decreased production of 5-MTHF (the active form of folate).
- Impaired homocysteine metabolism, leading to elevated homocysteine levels.
- Reduced availability of methyl groups for key biochemical processes.
Methylation is crucial for various bodily functions, including the regulation of thyroid hormone production and detoxification of environmental toxins that can harm the thyroid.
2. How MTHFR Affects Thyroid Function
a. Thyroid Hormone Activation
Thyroid hormone production begins with the secretion of thyroxine (T4) by the thyroid gland. T4 is converted into the active hormone triiodothyronine (T3) primarily in the liver and kidneys. This conversion depends on adequate methylation, making efficient MTHFR function essential.
- Impact of MTHFR mutations: Impaired methylation can reduce the conversion of T4 to T3, leading to symptoms of hypothyroidism despite “normal” T4 levels. Patients may present with fatigue, weight gain, cold intolerance, and brain fog due to insufficient active thyroid hormone.
b. Stress and Reverse T3 (rT3)
Stress is a known trigger for increased production of reverse T3 (rT3), an inactive form of T3. MTHFR mutations can exacerbate this process:
- Individuals with MTHFR mutations may have lower levels of methylated B vitamins (like B12 and folate), which are necessary for managing stress.
- Stress-induced cortisol surges increase rT3, further reducing the availability of active thyroid hormone.
c. Detoxification and Thyroid Toxins
The thyroid gland is highly sensitive to environmental toxins such as fluoride, bromide, chlorine, and heavy metals. Efficient detoxification, a process dependent on methylation, helps mitigate this exposure.
- Impact of impaired methylation: Poor detoxification increases oxidative stress and inflammation in the thyroid gland, which can exacerbate conditions like Hashimoto’s thyroiditis and Graves’ disease.
d. Methylation and Thyroid Autoimmunity
MTHFR mutations are commonly associated with higher levels of homocysteine, a pro-inflammatory compound. Elevated homocysteine levels can:
- Increase oxidative stress, damaging thyroid tissues.
- Trigger autoimmune responses, leading to conditions like Hashimoto’s thyroiditis or Graves’ disease.
- Reduce the availability of glutathione, a powerful antioxidant required to protect the thyroid from inflammation and autoimmune damage.
Want to dive deeper into how to treat thyroid disease with genomics? Join us at the Advanced Techniques for Autoimmune and Thyroid Workshop
3. Key Nutrients for MTHFR and Thyroid Function
Optimizing thyroid health in individuals with MTHFR mutations requires addressing both methylation and thyroid-specific nutrient needs. Some critical nutrients include:
a. Folate (Methylfolate)
- Essential for methylation and DNA synthesis.
- Avoid synthetic folic acid, which may not be processed effectively in individuals with MTHFR mutations.
b. Vitamin B12 (Methylcobalamin)
- Supports methylation and red blood cell production.
- Deficiencies can exacerbate fatigue and hypothyroid symptoms.
c. Selenium
- Crucial for converting T4 to T3.
- Reduces thyroid inflammation by supporting glutathione production.
d. Iodine
- Required for thyroid hormone synthesis.
- Must be used cautiously, especially in autoimmune thyroid conditions.
e. Zinc
- Supports thyroid hormone production and immune function.
f. Vitamin D
- Modulates immune function and reduces autoimmune activity in the thyroid.
g. Riboflavin (Vitamin B2)
- A cofactor for MTHFR enzyme activity and crucial for methylation.
4. MTHFR and Thyroid Disorders: Clinical Insights
a. Hypothyroidism
In hypothyroidism, MTHFR mutations can impair the methylation processes required for converting T4 to T3, compounding the symptoms of fatigue, depression, and weight gain. Supporting methylation with active B vitamins, selenium, and iodine can improve thyroid function.
b. Hashimoto’s Thyroiditis
This autoimmune condition often coincides with elevated homocysteine and inflammation. Managing MTHFR mutations with a gluten-free diet, methylated B vitamins, and anti-inflammatory strategies can reduce thyroid antibodies and support immune balance.
c. Graves’ Disease
In Graves’ disease, overactive thyroid function can accelerate methylation demands, depleting essential nutrients like B12 and folate. Tailored supplementation can help restore balance.
d. Postpartum Thyroiditis
MTHFR mutations may increase susceptibility to postpartum thyroid issues due to the high demand for methylation during pregnancy. Supporting methylation pathways before, during, and after pregnancy is crucial.
5. Practical Steps to Support MTHFR and Thyroid Health
- Test and Monitor:
- Check for MTHFR mutations through genetic testing.
- Regularly monitor thyroid hormone levels (TSH, T4, T3, rT3, and antibodies).
- Assess homocysteine levels and key nutrient statuses (selenium, iodine, B12, etc.).
- Personalized Supplementation:
- Use methylfolate and methylcobalamin to optimize methylation.
- Address selenium, zinc, and iodine deficiencies as needed.
- Dietary Changes:
- Follow an anti-inflammatory, nutrient-dense diet.
- Eliminate gluten, which can exacerbate autoimmune thyroid conditions.
- Reduce Toxin Exposure:
- Avoid fluoride and bromide in water and food.
- Opt for organic produce to minimize pesticide exposure.
- Manage Stress:
- Practice stress reduction techniques like mindfulness and yoga.
- Support adrenal health to regulate cortisol levels.
6. Conclusion
The intricate connection between the MTHFR gene and thyroid function underscores the importance of a personalized approach to thyroid health. Addressing methylation deficits, managing stress, and optimizing nutrient levels can significantly improve outcomes for individuals with thyroid conditions. If you suspect MTHFR mutations are contributing to your thyroid issues, working with a knowledgeable practitioner can help you develop a targeted strategy to restore balance and vitality.
By understanding the role of MTHFR in thyroid health, you can take proactive steps to support your thyroid and overall well-being.
Want to dive deeper into how to treat thyroid disease with genomics? Join us at the Advanced Techniques for Autoimmune and Thyroid Workshop