We learned previously that there are differences between folic acid and methyl folate when they are taken by pregnant women. New scientific studies reveal more of the risks of folic acid intake in pregnancy. Additionally, even though adequate folate intake is necessary in the safety and health of pregnancy, new research shows that folic acid at higher doses may be harmful to the human body particularly in pregnant women. This blog gives current updates to the risks of folic acid, and the risks of excessive folate intake in pregnancy; as well as the correct ways to handle all of these.
1. Risks of Folic Acids
Scientific studies show clearly that unsuitable folic acid intake in moms can change DNA methylation levels and gene expression in babies. One of the studies was performed in rats because it is impossible to be done in humans because of ethical reasons. The study shows that there are differences between folic acid intake during different time points or stages in pregnancy. For example, folic acid intake in early stages like the 2nd or 3rd week can increase liver folate remarkably. But when it is taken in late stages of pregnancy, it may cause incredibly lower DNA methylation levels in the brain. Surprisingly, when folic acid is taken throughout the pregnancy, the Brain DNA methylation reaches the lowest levels.
This study indicates that we need to re-consider carefully when supplying folic acid to our babies, and we need to avoid causing genomic and epigenetic changes.1 It suggests that supplying folic acid in the 1st week and extending it to the 2nd week of pregnancy may be enough for neuroprotection in the brain. It also suggests that folic acid supplementation in late stages of or throughout pregnancy may not be a good idea because it may cause unwanted changes in genome DNA methylation.
A different study conducted in humans confirms the opinions above but from a different angle. This study was trying to find out the causes of smaller foetuses, and changes in smaller foetus related genes such as H19 and MEST. In those moms who took folic acid during their conception, the methylation levels of the gene H19 were remarkably higher. This is not good, because higher level of methylation in the gene H19 has been confirmed to cause smaller foetuses. Moreover, this impact of folic acid intake during conception causing smaller foetuses is more obvious in boys than girls.
Most significantly, a report from Johns Hopkins Bloomberg School of Public Health investigates data from 1391 moms and their children, in the Boston Birth Cohort between 1998 and 2013 and followed for several years. It shows that 1 in 10 of the moms took excessive amount of folic acid, and 6 in 100 of the moms took excessive amount of vitamin B12. Those new moms with four times higher than adequate amount of folic acid doubled the risk of autism in their babies. In those new mums with both folic acid and B12 overdoses, the risk of autism in their babies increased 17.6 times.
In the above reports, folic acid was targeted. But since methyl folate or 5-MTHF has not been used as comparison we don’t know what the exact impact would have been with 5-MTHF. But we do know that large doses of 5-MTHF do not increase in the blood anywhere near levels of unmetabolised folic acid. What these studies are telling us is that we need to be cautious of high levels of folic acid as we are not only getting this in our diet but also our supplementation.
2. Risks of Excessive Folate Intake
In the past decades, we reached an important understanding that sufficient supplementation of folate reduces neural tube defects and other health risks in pregnancy. Sufficient folate supplement has been given through fortified foods and diet supplements. But the attention to overdose or excessive folate intake in pregnancy is rarely studied, and thus related information is limited. Currently, scientific studies are being conducted in an attempt to defining high folate dose and set up guidelines for folate intake. In May 2015, an expert panel was set up to examine current research, and to define that there are at least four side-effects from folic acid overdose, which are allergy, cognition disorders, cancer, and inflammation-like disorders such as diabetes. Among these side effects, cognition disorders is in conjunction with vitamin B12 deficiency (which can be masked by folic acid supplementation).
It seems that vitamin B12 deficiency makes the side-effect of excessive folate worse. Studies disagree with a statement from the WHO that “high folic acid intake has not reliably been shown to be associated with negative health effects”; instead, it is shown strongly that overdose of folic acid is not always safe particularly in certain populations, such as different ages, ethnic groups, and genetic background.
For example, in elderly populations, higher homocysteine and methylmalonic acid levels in plasma is related to clinical anaemia, cognitive impairment, and signs of vitamin B12 deficiency. These studies were conducted in Australia and the U. S. Furthermore, the side effects of folic acid overdose are not limited to elderly or B12 deficiency. A study group in India shows that high folic acid levels in red blood cells of pregnant women is linked to higher insulin resistance in babies, and it may increase the risk of diabetes in later lives. Another study group in the U. S. shows that folic acid intake by pregnant women increase the risk of tumour 4-fold higher in their babies.
A study conducted in China shows that folic acid supply in the first trimester (week 1 – 12) is related to an increased risk of gestational diabetes. This happens more often in those pregnant women with a BMI higher than 25 kg/m2 before pregnancy. The gestational diabetes is not seen in those pregnant women who took folic acid before their pregnancy or in the second trimester (week 13 – 28) alone.
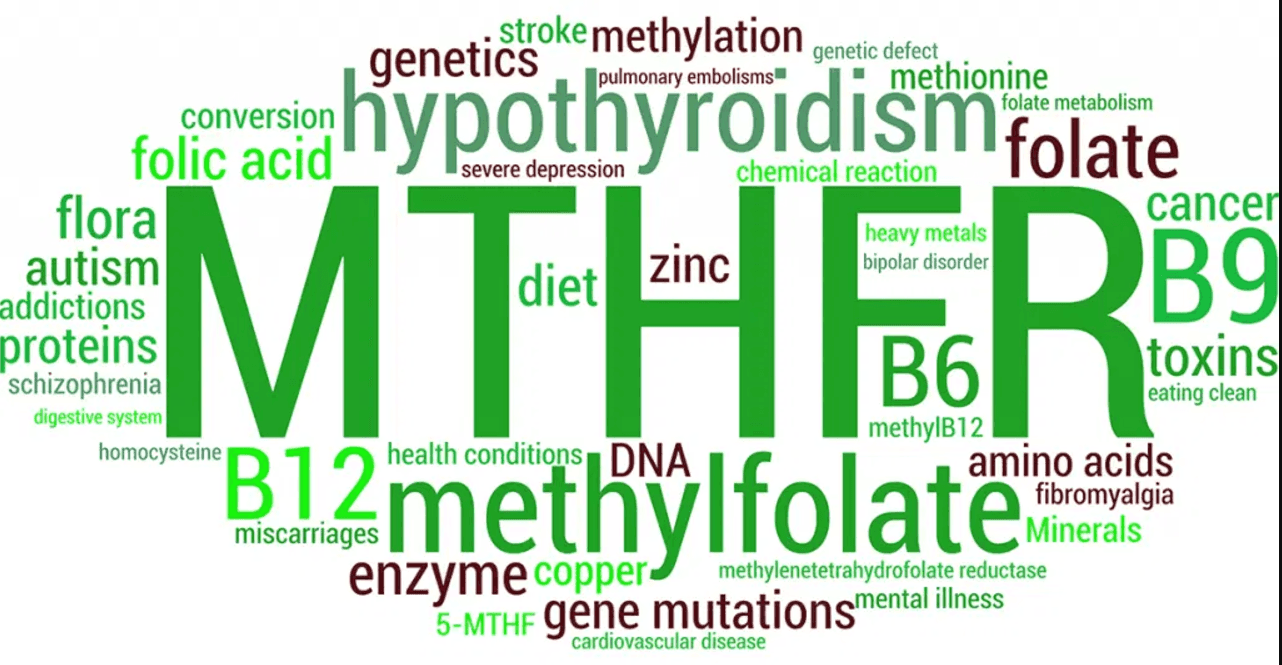
Why excessive folic acid supplementation causes the above healthy issues is not clear? We may hypothesise the following. Firstly, if we have an MTHFR or other folate related gene deficiencies then folic acid is not being converted to L-5MTHF and therefore is not being utilised. Secondly if we have a deficiency in Vitamin B12 then we may not be utilising our folate efficiently and this may cause different pathogenic processes.4 Thirdly, excessive folic acid may cause higher level of unmetabolised folate in the plasma, and unmetabolised folate is known to cause health issues. Fourthly, there are differences between supplements of folic acid, folinic acid and methyl folate (5-MTHF), and these differences are described below.
3. Current Understanding of Folic Acid, Folinic Acid & Methyl Folate in Pregnancy
So the studies are confusing because again we see terminology used differently. Some researchers say folate when they mean folic acid and you do not know what has been used until you analyse the data closely. If we only look at folic acid for a second, we know that supplying folic acid in the 1st and 2nd weeks of pregnancy may be enough for neuroprotection in the brain but not late stage.1 In addition, it is also found that folic acid supply in the first trimester (week 1 – 12) is related to an increased risk of gestational diabetes.9 Further study will be needed to clarify this, however we may take this as a warning that not to overdose folate in pregnancy, particularly in those women with higher risks of B12 deficiency, diabetes, and cancer.
Recently, there are intensive discussions about the differences between folic acid, folinic acid and methyl folate (5-MTHF), and their impact on pregnancy. As mentioned above, folic acid bears higher risks of cancer and higher level of unmetabolised folic acid in the blood; which may cause unwanted changes in genome DNA methylation particularly in the brain; furthermore it may cause a higher risk of autism in babies; and thus is detrimental to pregnant women. But how about folinic acid and 5-MTHF?
Folinic acid, unlike folic acid, is a naturally occurring folate. Due to its natural occurring features, folinic acid can be used to rescue low folate and its derived health issues such as enabling normal cell growth in low folate supply. , In addition, 5-MTHF is considered safer compared to folic acid, because 5-MTHF is a natural form of folate and induces higher folate concentration within a shorter time in the blood stream; and it causes much lower levels of unmetabolised folic acid in the blood compared to folic acid. And thus the risk of overdose of 5-MTHF is much lower than folic acid.
Summary
In summary, adequate folate intake is necessary in pregnancy, but its dose and form needs to be well controlled. Excessive folic acid intake is confirmed to cause higher risks of allergy, cognition disorders, cancer, diabetes, higher rates of autism and other health issues in both pregnant women and their babies. So for those with mutations in the folate pathway like Folate Receptor 2 genes, MTHFD1, MTHFD1L, MTHFS, and MTHFR and in the B12 genes MTR and MTRR we are much safer using either folinic or L-5MTHF. L-5MTHF particularly as it’s a natural form of folate and its risk of overdose is much lower than folic acid for pregnant women.
If you have the MTHFR gene and would like to safely prepare you and your partner’s body for conception and pregnancy, my MTHFR and Preconception course is a complete resource for a healthy and thriving pregnancy. Learn more by clicking here.
Bibliography
[1] Ly A, Ishiguro L, Kim D, Im D, Kim SE, Sohn KJ, Croxford R, Kim YI. Maternal folic acid supplementation modulates DNA methylation and gene expression in the rat offspring in a gestation period-dependent and organ-specific manner. J Nutr Biochem. 2016 Jul; 33: 103-10. PMID: 27152636
[2] Qian YY, Huang XL, Liang H, Zhang ZF, Xu JH, Chen JP, Yuan W, He L, Wang L, Miao MH, Du J, Li DK. Effects of maternal folic acid supplementation on gene methylation and being small for gestational age. J Hum Nutr Diet. 2016 May 27. PMID: 27230729
[3] News Release. Too much folate in pregnant women increases risk for autism, study suggests. Johns Hopkins Bloomberg School of Public Health. Retrieved from http://www.jhsph.edu/news/news-releases/2016/too-much-folate-in-pregnant-women-increases-risk-for-autism-study-suggests.html
[4] Boyles AL, Yetley EA, Thayer KA, Coates PM. Safe use of high intakes of folic acid: research challenges and paths forward. Nutr Rev. 2016 Jul; 74(7): 469-74. PMID: 27272334
[5] Selhub J, Rosenberg IH. Excessive folic acid intake and relation to adverse health outcome. Biochimie. 2016 Jul; 126:71-8. PMID: 27131640
[6] Moore EM, Ames D, Mander AG, Carne RP, Brodaty H, Woodward MC, Boundy K, Ellis KA, Bush AI, Faux NG, Martins RN, Masters CL, Rowe CC, Szoeke C, Watters DA. Among vitamin B12 deficient older people, high folate levels are associated with worse cognitive function: combined data from three cohorts. J Alzheimers Dis. 2014; 39(3): 661-8. 24246419
[7] Miller JW, Garrod MG, Allen LH, Haan MN, Green R. Metabolic evidence of vitamin B-12 deficiency, including high homocysteine and methylmalonic acid and low holotranscobalamin, is more pronounced in older adults with elevated plasma folate. Am J Clin Nutr. 2009 Dec; 90(6): 1586-92. PMID: 19726595
[8] Yajnik CS, Deshpande SS, Jackson AA, Refsum H, Rao S, Fisher DJ, Bhat DS, Naik SS, Coyaji KJ, Joglekar CV, Joshi N, Lubree HG, Deshpande VU, Rege SS, Fall CH. Vitamin B12 and folate concentrations during pregnancy and insulin resistance in the offspring: the Pune Maternal Nutrition Study. Diabetologia. 2008 Jan; 51(1): 29-38. PMID: 17851649
[9] Orjuela MA, Cabrera-Muñoz L, Paul L, Ramirez-Ortiz MA, Liu X, Chen J, Mejia-Rodriguez F, Medina-Sanson A, Diaz-Carreño S, Suen IH, Selhub J, Ponce-Castañeda MV. Risk of retinoblastoma is associated with a maternal polymorphism in dihydrofolatereductase (DHFR) and prenatal folic acid intake. Cancer. 2012 Dec 1; 118(23): 5912-9. PMID: 22648968
[10] Zhu B, Ge X, Huang K, Mao L, Yan S, Xu Y, Huang S, Hao J, Zhu P, Niu Y, Tong S, Tao F. Folic Acid Supplement Intake in Early Pregnancy Increases Risk of Gestational Diabetes Mellitus: Evidence From a Prospective Cohort Study. Diabetes Care. 2016 Mar; 39(3): e36-7. PMID: 26822325
[11] Bailey RL, Mills JL, Yetley EA, Gahche JJ, Pfeiffer CM, Dwyer JT, Dodd KW, Sempos CT, Betz JM, Picciano MF. Unmetabolized serum folic acid and its relation to folic acid intake from diet and supplements in a nationally representative sample of adults aged > or =60 y in the United States. Am J Clin Nutr. 2010 Aug; 92(2): 383-9. PMC2904036
[12] Zhu WY, Melera PW. Metallothionein is overexpressed by hamster fibroblasts selected for growth in 15 pm folinic acid and provides a growth advantage in low folate. Cancer Res. 1999 Sep 1; 59(17): 4194-9. PMID: 10485453
[13] Ramaekers VT, Thöny B, Sequeira JM, Ansseau M, Philippe P, Boemer F, Bours V, Quadros EV. Folinic acid treatment for schizophrenia associated with folate receptor autoantibodies. Mol Genet Metab. 2014 Dec; 113(4): 307-14. PMID: 25456743
[14] Venn BJ, Green TJ, Moser R, Mann JI. Comparison of the effect of low-dose supplementation with L-5-methyltetrahydrofolate or folic acid on plasma homocysteine: a randomized placebo-controlled study. Am J Clin Nutr. 2003 Mar; 77(3): 658-62. PMID: 12600857
[15] Prinz-Langenohl R, Brämswig S, Tobolski O, Smulders YM, Smith DE, Finglas PM, Pietrzik K. [6S]-5-methyltetrahydrofolate increases plasma folate more effectively than folic acid in women with the homozygous or wild-type 677C–>T polymorphism of methylenetetrahydrofolate reductase. Br J Pharmacol. 2009 Dec; 158(8): 2014-21. PMCID: PMC2807663
[16] Bailey RL, Mills JL, Yetley EA, Gahche JJ, Pfeiffer CM, Dwyer JT, Dodd KW, Sempos CT, Betz JM, Picciano MF. Unmetabolized serum folic acid and its relation to folic acid intake from diet and supplements in a nationally representative sample of adults aged > or =60 y in the United States. Am J Clin Nutr. 2010 Aug; 92(2): 383-9. PMC2904036
[17] Choi JH, Yates Z, Veysey M, Heo YR, Lucock M. Contemporary issues surrounding folic Acid fortification initiatives. Prev Nutr Food Sci. 2014 Dec; 19(4): 247-60. PMCID: PMC4287316