What do bones and the sun have in common? Vitamin D, of course. Discovered in 1928 by Adolf Windaus (famously known German scientist who opposed the Nazis), vitamin D is a key component of good health (1). However, you might be shocked to learn that vitamin D deficiency (VDD) is a major unrecognized public health problem - over 1 billion people around the world are lacking adequate levels of vitamin D (2). Up to 50% of the world have vitamin D insufficiency. Why are so many people lacking vitamin D and why is it so important? Read on to find out more.
What is vitamin D and why is it so important?
There are 2 main types of vitamin D that we get from our food – ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Vitamin D2 is present in sun-exposed mushrooms, while vitamin D3 is found in foods such as eggs, fish, cod liver oil, and beef liver. We’ll talk more about these forms of vitamin D later.
Vitamin D is an essential vitamin that is most popularly known to maintain healthy, strong bones by involving calcium metabolism. Without vitamin D, only 10-15% of calcium and 60% of phosphorus (another essential mineral in bone health) sources that we get from our diet are absorbed (3).
Did you know that vitamin D is also responsible for much more than that?
- Preventing cancer – several types of cancer including colon, breast, lung, pancreatic, prostate, and stomach cancer have all been linked to low vitamin D levels. Vitamin D is thought to influence the entire process of cancer formation, from the first, tiny cancer cell, cancer growth, and spread of cancer (4).
- Boosting the immune system – low vitamin D levels make our bodies more prone to infections, especially those involving our respiratory system (the common cold, tuberculosis) (5). Having low vitamin D levels may even put someone more at risk of developing severe COVID-19 infection due to the body being in a more pro-inflammatory state (6). VDD also contributes to several autoimmune diseases such as Crohn’s disease, autoimmune thyroid disease, multiple sclerosis, rheumatoid arthritis, and type 1 diabetes mellitus (5).
- Protecting heart health – Large studies have linked hypertension and ischemic heart disease to VDD (7).
- Preserving mental health and cognition – Depression is associated with low vitamin D levels (8). What’s more, dementias caused by Alzheimer’s and Parkinson’s disease may be related to chronically low vitamin D levels (9).
How our body makes vitamin D
Vitamin D is aptly known as the ‘Sun Vitamin’ because our bodies (specifically our skin) can turn sunlight into a vitamin D precursor. We also get vitamin D that’s absorbed from the gut from the food that we eat. Have a look at the diagram below:
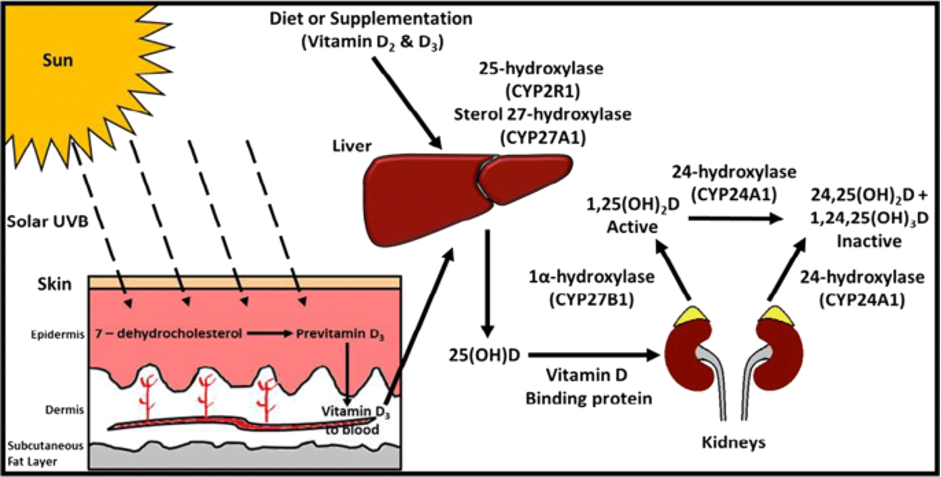
Figure 1: Vitamin D Metabolism. Image from: McCartney, D.M., O’Shea, P.M., Faul, J.L. et al. Vitamin D and SARS-CoV-2 infection—evolution of evidence supporting clinical practice and policy development. Ir J Med Sci (2020). https://doi.org/10.1007/s11845-020-02427-9
The forms of vitamin D from skin and food first must be activated in the liver in a process known as hydroxylation. The liver turns vitamin D to 25-hydroxyvitamin D (25OHD, or calcidiol). However, calcidiol isn’t the active form of vitamin D, and requires another hydroxylation in the kidney to finally become 1,25-dihydroxyvitamin D (1,25OH2D, or calcitriol, the active form of vitamin D.
Calcitriol goes on to increase calcium and phosphate absorption in the small intestine and kidneys. It also acts directly on the bone and interacts with the parathyroid gland (4 important glands in your neck that are crucial for calcium metabolism) to regulate calcium levels in the body.
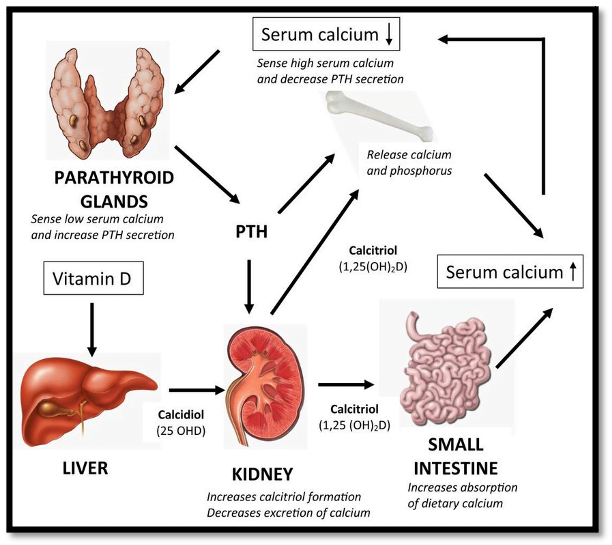
Figure 2: Calcium, parathyroid gland, and vitamin D interactions. Image from: Ballegooijien HV. The role of vitamin D and parathyroid hormone in cardiovascular health. May 2014. Available from: DOI: 10.13140/RG.2.2.22269.36321
For calcitriol to work in the body, it needs to bind to a vitamin D receptor (VDR) that is expressed on the cell nuclei (the control centre of the cell). VDR is found in many different cells in the body – which explains the multitude of effects that vitamin D has on various systems. Calcitriol-bound VDR forms another complex with the retinoid X receptor (RXR). Together, this molecule can control gene expression directly.
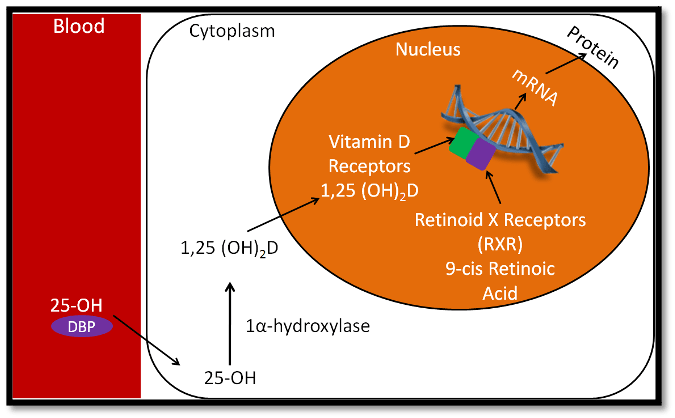
Figure 3: The interaction between calcitriol, vitamin D receptors and genes. Image from: https://courses.lumenlearning.com/suny-nutrition/chapter/12-15-vitamin-d-receptor/
Keep these pathways in mind – they’re important when we delve into the genetics behind vitamin D metabolism.
How much vitamin D do we need?
Interestingly, calcidiol levels, not calcitriol levels, are the best indicator of vitamin D stores in the body (10). You need to have levels of more than 30ng/mL (75nmol/L) of calcidiol to have enough vitamin D. Levels between 20 – 30ng/mL (50-75nmol/L) are considered vitamin D insufficiency, while levels below 20ng/mL (50nmol/L) are considered vitamin D deficiency (2).
Who are at risk of vitamin D deficiency?
Why are so many people lacking vitamin D? Well, this could be due to a combination of many things, including having a lower than usual intake over a long period of time (more common in those with lactose intolerance, and in ovo-vegetarians and vegans), those with poor ability to absorb or create vitamin D, or those with limited sunlight exposure.
- Breastfed infants – human milk alone does not usually provide enough vitamin D. The American Academy of Paediatrics recommend that exclusively and partially breastfed infants are given 10mcg (400IU) a day of vitamin D supplements until they’re able to drink at least 1L of vitamin D-fortified formula a day (11). Mothers should be careful to get enough vitamin D while breastfeeding as vitamin D content in breastmilk is related to mom’s status (11).
- Older adults – As we age, the skin loses its ability to efficiently synthesize vitamin D. Coupled with the fact that this population is more likely to spend time indoors and have less intake of vitamin D, older adults are more at risk of VDD (3).
- Those with limited sun exposure
- Darker skinned individuals – Those with naturally dark skin require 3 – 5 times longer sun exposure to get the same amount of vitamin D compared to lighter skinned individuals due to larger amounts of melanin in the skin (3).
- Fat malabsorption syndromes – In order for vitamin D to be absorbed, it needs to bind to dietary fat. Those who have trouble absorbing fat may need vitamin D supplements (3). Conditions like cystic fibrosis and Crohn’s disease are some examples of fat malabsorption syndromes. Similarly, those who have undergone gastric bypass surgeries may be vitamin D deficient if parts of the small intestine responsible for absorbing fat are cut out.
- Obese individuals – Having a BMI ≥ 30kg/m2 is associated with VDD.
- Chronic kidney disease – people with chronic kidney disease have lower vitamin D levels than healthy individuals despite getting the same amount of sun. High blood urea levels, decreased food intake, and skin hyperpigmentation are some reasons that cause VDD in this population (12).
Do you, or one of your loved ones, fall into any one of these categories? Read on to learn more about what happens if we don’t get enough vitamin D, and what we can do to avoid VDD.
What happens when we don’t get enough vitamin D?
Children who don’t get enough vitamin D are at risk of getting rickets, a condition that causes soft, weak bones and severe deformities. VDD causes muscle weakness and bone pain as well, and adults may complain of discomfort in the lower back, pelvis, and legs. Muscle weakness leads to a higher risk of falls and fractures (2).
Do our genes influence vitamin D status?
Genetics dictate a significant chunk of our physiological make up. No two people are exactly the same. This applies for everything from your hair colour, the amount of serotonin in our brains – and you guessed it – how your body metabolizes vitamin D.
As shown in Figure 1, there are a number of enzymes that are involved in how the body handles vitamin D. Having too much – or too little – of these enzymes sets off a cascade of reactions that ultimately influence vitamin D stores.
Genes that contain instructions for vitamin D-related enzymes (and everything else in the body) can sometimes have minor variations – called single nucleotide polymorphisms (SNPs). Scientists have discovered that certain SNPs occur more commonly in the population and have studied the effects of these SNPs on vitamin D metabolism.
CYP27B1 enzyme (1α-hydroxylase enzyme)
The CYP27B1 enzyme is responsible for converting calcidiol to calcitriol in the kidneys. Interestingly, the CYP27B1 is found in several other tissues besides the kidney, which could explain why vitamin D affects so many other organ systems.
Some CYP27B1 SNPs have been linked to a higher risk of getting type 1 diabetes (CYP27B1 −1260 and +2838) and colorectal cancer (rs10877012) (13, 14). The rs10877012 polymorphism however, has also been found to make its carriers more responsive to vitamin D supplements (meaning that these individuals would have higher vitamin D levels compared to non-carriers when both are given the same amounts of vitamin D supplements)(15).
Vitamin D Receptor
Like the CYP27B1 enzyme, the VDR is ubiquitously expressed in the human body including the heart, skin, immune system, and fat cells (16). It is estimated that up to 11,000 genes are under direct or indirect control of the VDR (16).
The rs1544410 (also known as Bsml) SNP has been shown to be related to higher triglyceride levels, while the rs7975232 (also known as Apal) SNP is associated to raised total cholesterol levels (17). Both these polymorphisms are also related to a higher risk of colorectal cancer (14).
The link between vitamin D SNPs and its effect on vitamin D metabolism has several implications. By analysing our genetic makeup, or testing for specific vitamin D-related SNPs, we may be able to tailor our supplementation exactly to our individual needs. However, commercial vitamin D SNP polymorphism testing is yet to be widely available.
Getting enough Vitamin D
Getting enough vitamin D is challenging based on natural food sources alone. Most people need a combination of enough sun exposure, vitamin D-fortified foods, and in some cases, supplementation. Let’s explore exactly what we can do to boost our vitamin D levels.
Daily vitamin D doses
Daily vitamin D needs are different depending on age and on whether a mother is breastfeeding. Figure 4 shows recommended doses based on the National Institutes of Health (United States):
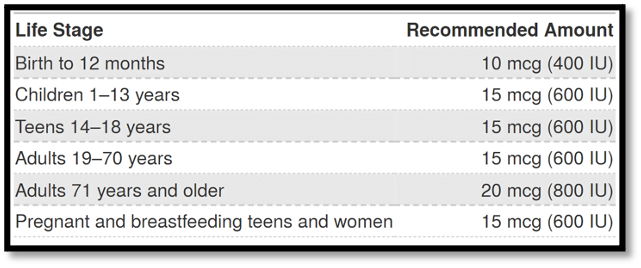
Figure 4: Daily recommended doses of vitamin D in non-vitamin D deficient individuals. Image from: https://ods.od.nih.gov/factsheets/VitaminD-Consumer/#h2.
However, if you are at risk of vitamin D deficiency, you may need much higher doses initially to help bring up those D levels. Tables 1 and 2 below show the daily recommended doses of vitamin D if you’re at risk of VDD:
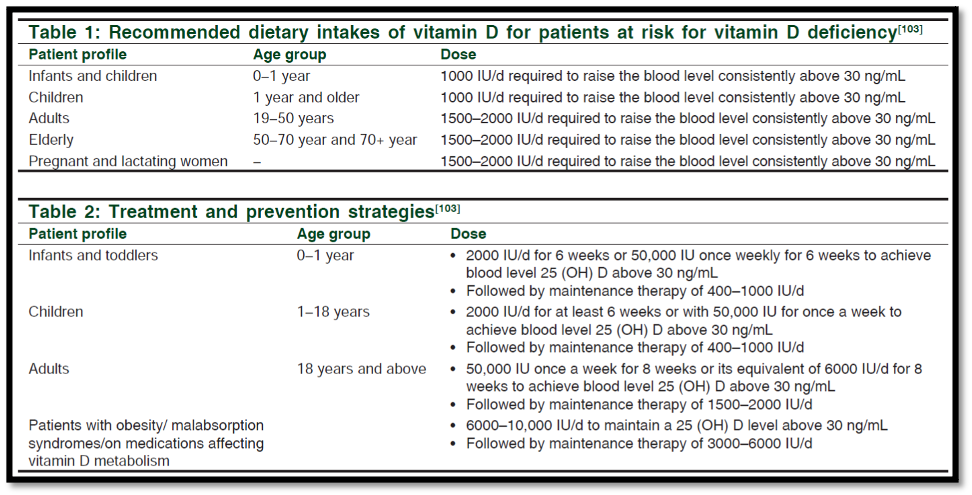
Tables 1 and 2: Recommended dietary intakes of vitamin D for patients at risk for vitamin D deficiency. Tables from: Nair R, Maseeh A. Vitamin D: The "sunshine" vitamin. J Pharmacol Pharmacother. 2012;3(2):118-126. doi:10.4103/0976-500X.95506.
Making sure we get enough vitamin D levels
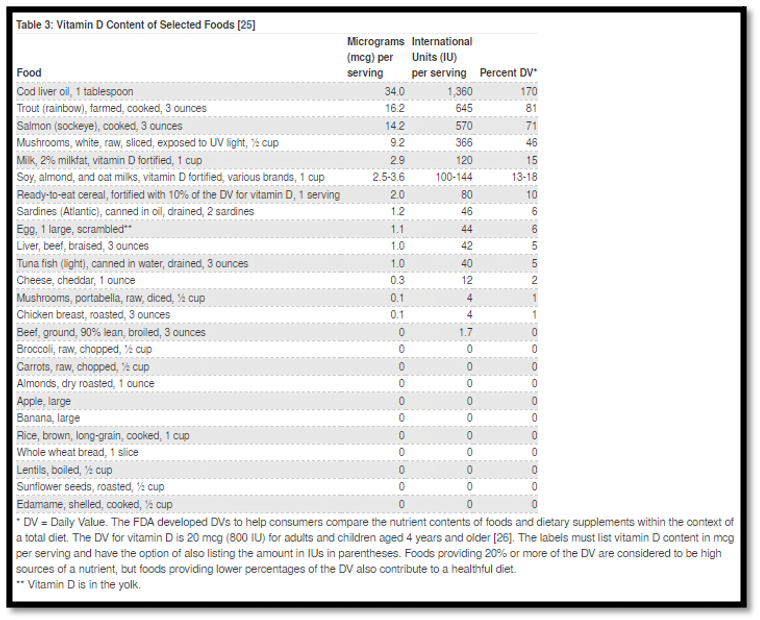
Table 3: Vitamin D Content of Selected Foods. Table from: https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#en56
- Eating the right foods. Given the pandemic proportions of vitamin D deficiency, several foods are pre-emptively fortified with vitamin D since the 1930s and 1940s (18). Foods that are commonly fortified are cereals and milk. Table 3 contains a comprehensive list of foods and their vitamin D content. A healthy, middle-aged adult would get enough vitamin D by just 1 serving of trout or 1 tablespoon of cod liver oil every day. In contrast, you’d have to eat 12 eggs a day to get the same amount of vitamin D!
- Getting enough sun. Type B UV radiation (UVB) is required for our skin to make vitamin D. Experts suggest that we need at least 5-30 minutes of sun exposure (between 10am – 4pm) either every day or at least twice a week to face, arms, hands, and legs without sunscreen. Being exposed to sunlight through a window doesn’t count, as the glass stops UVB. Bear in mind that older and darker skinned individuals make less vitamin D through sun exposure even if they’re under the sun for the same amount of time as lighter skinned individuals.
- Vitamin D supplements. Vitamin D supplements are available in the forms of vitamin D2, D3, and calcidiol (also known as calcifediol)(19). Of the three, calcidiol is the most effective in raising vitamin D levels, followed by vitamin D3, then vitamin D2.
Can we get too much vitamin D?
Yes, you can! Known as hypervitaminosis D, too much vitamin D causes nausea, vomiting, muscle weakness, confusion, pain, loss of appetite, dehydration, excessive urination and thirst, and kidney stones. This usually happens in those who have too much in their vitamin D supplements. You cannot get too much vitamin D from sun exposure.
Certain medications like statins, steroids, and thiazides may interact with vitamin D supplements, either by reducing or dangerously enhancing vitamin D absorption. Talk to your physician about vitamin D supplementation, especially if you’re on these medications.
Vitamin D: A truly vital amine
Like the sun, vitamin D is a critical supporter of life. Don’t let yourself get deficient - make sure that you’re getting enough sun, vitamin D-rich food, and supplements. At the same time - too much of a good thing is bad – beware of hypervitaminosis D.
If you would like to learn more about Vitamin D, why not join our webinar:
1. Wolf G. The Discovery of Vitamin D: The Contribution of Adolf Windaus. The Journal of Nutrition. 2004;134(6):1299-302.
2. Paula Bordelon MVG, Robert Langan. Recognition and Management of Vitamin D Deficiency. American Family Physician. 2009;80(8):6.
3. Nair R, Maseeh A. Vitamin D: The "sunshine" vitamin. J Pharmacol Pharmacother. 2012;3(2):118-26.
4. Jeon SM, Shin EA. Exploring vitamin D metabolism and function in cancer. Exp Mol Med. 2018;50(4):1-14.
5. Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020;12(7).
6. Weir EK, Thenappan T, Bhargava M, Chen Y. Does vitamin D deficiency increase the severity of COVID-19? Clin Med (Lond). 2020;20(4):e107-e8.
7. Brondum-Jacobsen P, Benn M, Jensen GB, Nordestgaard BG. 25-hydroxyvitamin d levels and risk of ischemic heart disease, myocardial infarction, and early death: population-based study and meta-analyses of 18 and 17 studies. Arterioscler Thromb Vasc Biol. 2012;32(11):2794-802.
8. Menon V, Kar SK, Suthar N, Nebhinani N. Vitamin D and Depression: A Critical Appraisal of the Evidence and Future Directions. Indian J Psychol Med. 2020;42(1):11-21.
9. Moretti R, Morelli ME, Caruso P. Vitamin D in Neurological Diseases: A Rationale for a Pathogenic Impact. Int J Mol Sci. 2018;19(8).
10. Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc. 2010;85(8):752-8.
11. Wagner CL, Greer FR. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122(5):1142-52.
12. Franca Gois PH, Wolley M, Ranganathan D, Seguro AC. Vitamin D Deficiency in Chronic Kidney Disease: Recent Evidence and Controversies. Int J Environ Res Public Health. 2018;15(8):1773.
13. Bailey R, Cooper JD, Zeitels L, Smyth DJ, Yang JH, Walker NM, et al. Association of the vitamin D metabolism gene CYP27B1 with type 1 diabetes. Diabetes. 2007;56(10):2616-21.
14. Vidigal VM, Silva TD, de Oliveira J, Pimenta CAM, Felipe AV, Forones NM. Genetic polymorphisms of vitamin D receptor (VDR), CYP27B1 and CYP24A1 genes and the risk of colorectal cancer. Int J Biol Markers. 2017;32(2):e224-e30.
15. Hu Z, Tao S, Liu H, Pan G, Li B, Zhang Z. The Association between Polymorphisms of Vitamin D Metabolic-Related Genes and Vitamin D3 Supplementation in Type 2 Diabetic Patients. J Diabetes Res. 2019;2019:8289741.
16. Saponaro F, Saba A, Zucchi R. An Update on Vitamin D Metabolism. Int J Mol Sci. 2020;21(18).
17. Karonova T, Grineva E, Belyaeva O, Bystrova A, Jude EB, Andreeva A, et al. Relationship Between Vitamin D Status and Vitamin D Receptor Gene Polymorphisms With Markers of Metabolic Syndrome Among Adults. Front Endocrinol (Lausanne). 2018;9:448.
18. Pilz S, März W, Cashman KD, Kiely ME, Whiting SJ, Holick MF, et al. Rationale and Plan for Vitamin D Food Fortification: A Review and Guidance Paper. Frontiers in endocrinology. 2018;9:373-.
19. Vaes AMM, Tieland M, de Regt MF, Wittwer J, van Loon LJC, de Groot L. Dose-response effects of supplementation with calcifediol on serum 25-hydroxyvitamin D status and its metabolites: A randomized controlled trial in older adults. Clin Nutr. 2018;37(3):808-14.